ONE OUT OF EIGHT MEN WILL HAVE PROSTATE CANCER AT SOME MOMENT
Fortunately, prostate cancer tends to grow slower than other types, which allows for several therapeutic options. In this post, I’ve gathered the most important info you need to know.
Table of Content
Some useful terms
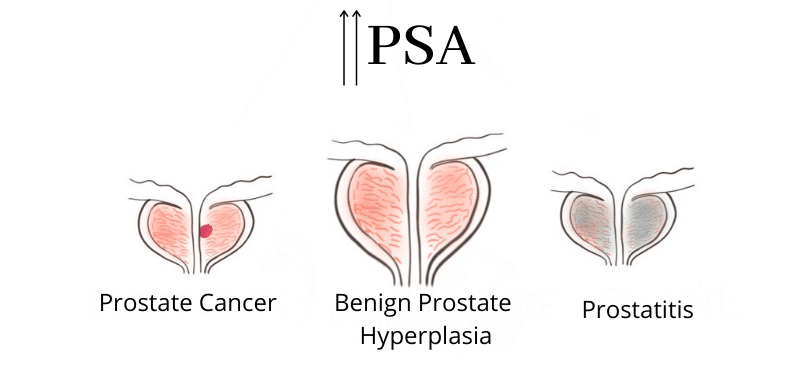
- PSA: Prostate Specific Antigen. It’s a protein in your blood. Its levels rise in cases of prostate cancer, but it is not specific: it’s also high in non-cancer conditions such as prostatitis and benign prostate hyperplasia (BPH).
- Benign prostate hyperplasia (BPH): when your prostate is diffusely enlarged. It‘s just large, with no cancer. It can cause similar symptoms to prostate cancer because it can compress the urethra, too.
- Gleason: the numeric system for the results of the biopsy. It goes from 6 (less aggressive) to 10 (very aggressive).
- PI-RADS: the numeric system that describes the results of the MRI. It goes from 1 (very unlikely to be cancer) to 5 (highly likely it will be cancer).
- Prostatectomy: surgical procedure to remove the prostate.
- Lymphadenectomy: surgery to remove affected pelvic lymph nodes.
Symptoms
It’s better to detect prostate cancer as early as possible. That way, treatment will be less aggressive and more effective.
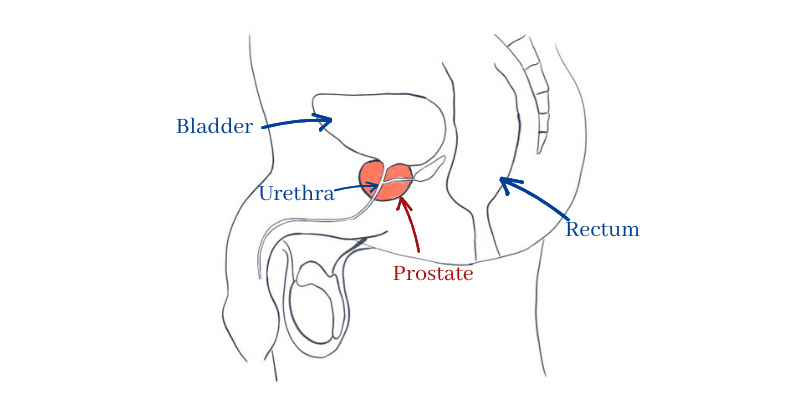
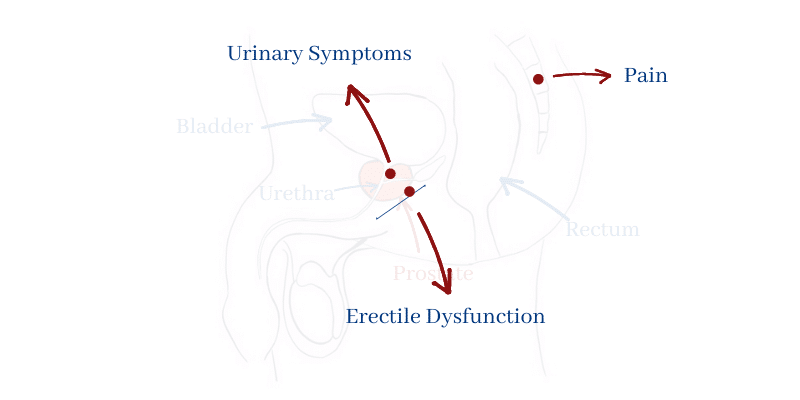
The problem is, though, that when the tumor is small it may not cause any symptoms. That’s because prostate cancer usually grows away from the urethra (the urine duct) and so it doesn’t cause any problems until it gets larger.
In other cases, the nodule is located centrally and it will compress the urethra early on, causing urinary symptoms. That’s good luck, in a way, because we can diagnose it earlier. For example, you’ll get a weak jet while peeing, or an urgency to pee right away. Some people can also notice blood in your pee or in your semen.
Finally, if the tumor has spread it can cause pain in your bones (bone metastases) or erectile dysfunction (if it spreads into the surrounding nerves).
If you want to read more about prostate cancer symptoms, click here.
How To Detect Prostate Cancer
PSA
PSA is the “prostate-specific antigen” and it’s produced by the prostate. So, the more prostatic tissue, the higher PSA.
Values above > 4 ng/ml are considered high.
It’s the first test used on a man with urinary symptoms, along with a rectal examination.
If the PSA levels are low, it’s unlikely that you have prostate cancer… But what if it’s high?
What does a high PSA mean?
A high PSA doesn’t always mean cancer. In fact, it’s more likely due to other entities such as benign prostate hyperplasia (BPH).
BPH is a benign enlargement of the prostate and it also increases PSA. It consists of a large prostate, but without cancer.
Prostatitis, an inflammation of the prostate, can also increase the PSA.
Prostate MRI
If PSA is high, the next step is usually a prostate MRI. MRI can detect suspicious nodules and it will also show where the nodules are. That way, the surgeon can then perform a guided biopsy, to get a sample.
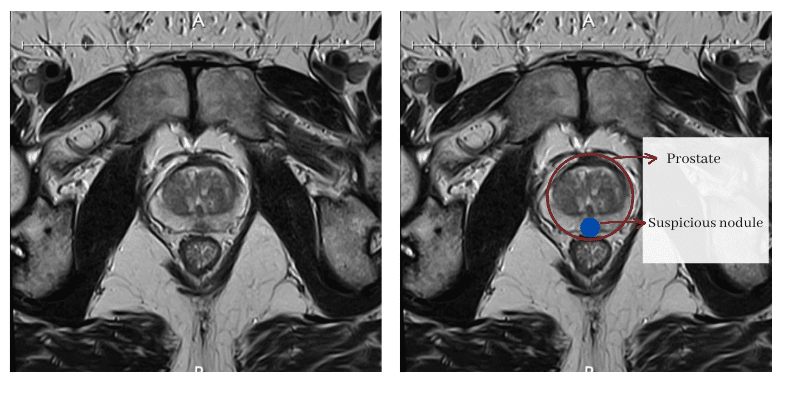
The MRI report includes a PI-RADS score consisting of a number from 1 to 5.
PI-RADS 1 means there is very little chance of cancer. PI-RADS 5 means there is a high chance of cancer.
Biopsy
A biopsy is a procedure to get several samples from your prostate. We do it with a special needle, usually through the wall of your rectum with the help of an ultrasound.
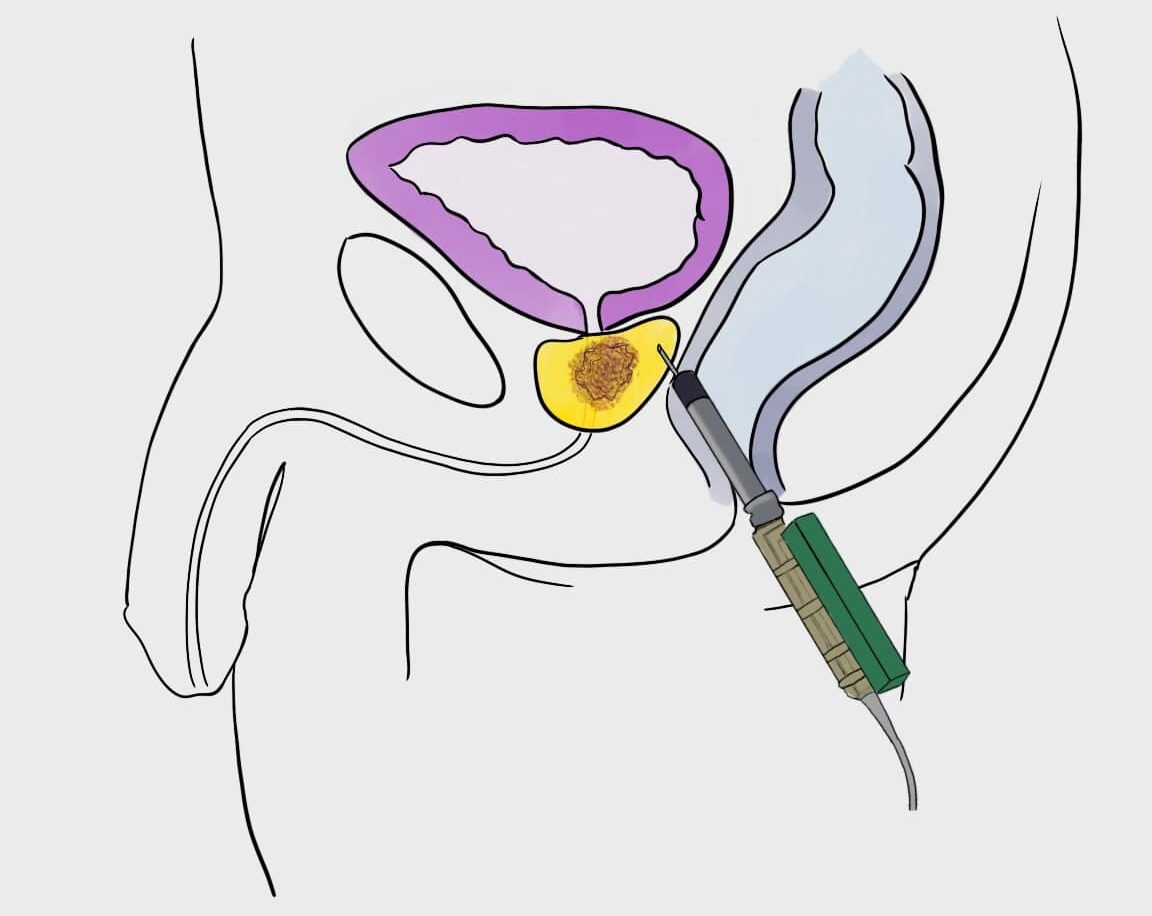
The urologist will take a sample from every section of the prostate and several more from the “ugly” areas detected on MRI.
After that, the pathologist will analyze the samples and make a report with the Gleason score, which goes from 6 to 10.
Gleason 6 means the cancer is not too aggressive and Gleason 10 means it is very aggressive. Aggressive tumors are more likely to spread and require more aggressive therapy.
How To Treat Prostate Cancer
There are many options that your urologist or oncologist will discuss with you. The main factor is: is the tumor localized or has it spread?.
If the tumor is localized
When the tumor hasn’t spread (no metastases), the most common option is a radical prostatectomy. That means removing the whole prostate through surgery.
There are two ways to do it, through open surgery or laparoscopic surgery. Nowadays, laparoscopic surgery is better because it causes less side effects.

If the tumor has spread to the we’ll need to remove them too. This is known as lymphadenectomy.
An alternative to surgery is brachytherapy. Brachytherapy consists of several tiny radioactive seeds that go inside your prostate. These seeds will release radiation continuously to the nearby tissues, destroying your tumor. In several cases, brachytherapy has proven to be equally effective than surgery. So, you’d get the same results with either one. You can read more about it here.
Sometimes, you may need radiotherapy after surgery, especially if the tumor has spread into the surrounding tissues (and sometimes we only find out after surgery). Read more here.
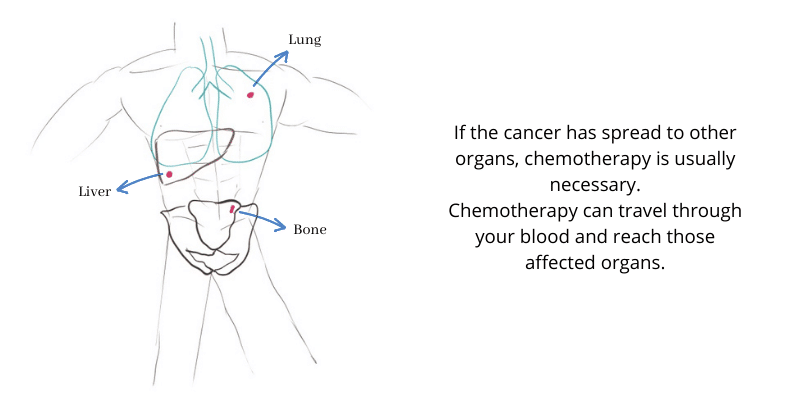
If the tumor has spread
When the tumor has spread, most patients will benefit from chemotherapy. Chemotherapy travels through your blood and kills distant malignant cells.
Sometimes, hormone therapy is also required. Hormone therapy counters the testosterone effect and prevents the tumor’s growth.
To read more about prostate cancer stages, click here.
Some Questions & Answers
-
Is It Hereditary?
It isn’t hereditary as in “you inherit from your father”. However, one of the most important risk factors for prostate cancer is your family predisposition. If members of your family (father, brothers) had it, your chances are higher.
Also, there are some known genetic mutations that predispose to it, like BCRA mutations.
-
Is It Contagious?
No, it isn’t. Not through sexual contacts nor any other way.
-
Will It Come Back?
It can’t be predicted exactly if cancer will recur after treating it. However, we can get an idea.
If the tumor was small and its Gleason score was low, chances are it won’t come back. Aggressive tumors will be more likely to come back.
To make sure, you will have to take the follow-up tests. That’s usually a PSA analysis every 6 months. If PSA remains low, then everything is ok.
Sometimes, you will also need a body CT or a bone scan to check for bone metastases.
Leave a Reply