Parkinson’s disease is best known for the tremors it causes. However, it can cause many other symptoms, and some of them are much more invalidating than tremors. For example, bradykinesia (slow motions), stiffness, and walking disorders. Let’s see all these symptoms, as well as how to treat it and how to diagnose it.
Table of content
What is Parkinson’s disease?
Parkinson’s disease is a neurological movement disorder. It causes tremors, but also stiffness, slow motions, walking disturbance… There are even other less known symptoms that don’t have anything to do with movement, like constipation, loss of smell…
Finally, it causes some symptoms like depression, delusions, and memory problems because it is a neurodegenerative disease.
It can affect anyone, but the risk is higher for men and older people (over 60 years old). There is a variant that affects young people called Young Onset Parkinson’s Disease (YOPD), which affects people younger than 50 years of age. You may know the example of Michael J. Fox, the famous actor who got Parkinson at the age of 29.
What’s the mechanism behind Parkinson’s disease?
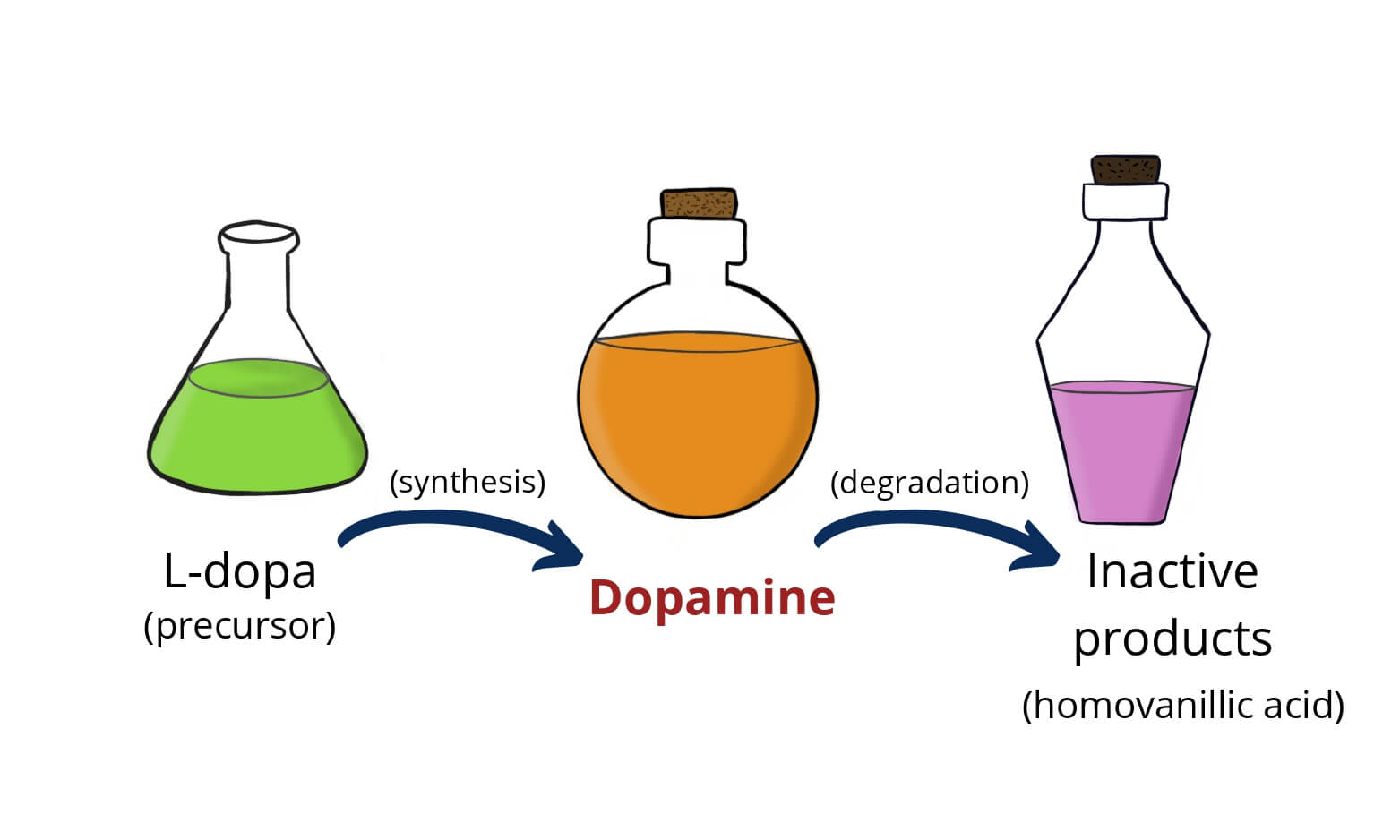
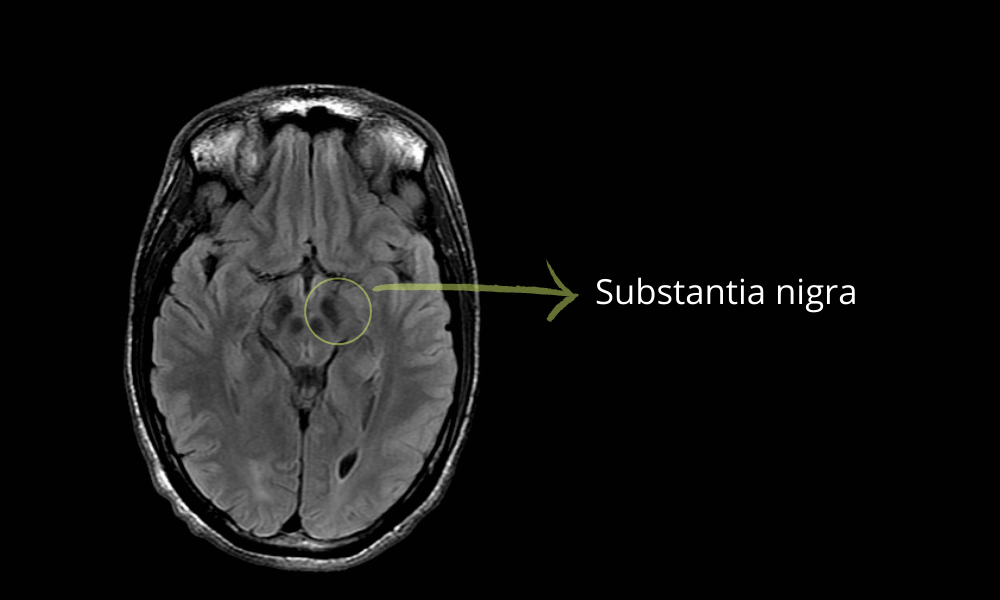
There is an area in the brain called the “substantia nigra“. It produces dopamine, using a precursor called L-DOPA. This substance, dopamine, has a role in controlling the body’s movement.
It makes sure our movements are precise. Then, some of the dopamine turns into norepinephrine, the main substance responsible for our sympathetic nervous system.
In Parkinson’s disease, the substantia nigra cells start to die and patients run out of dopamine. This causes motor symptoms, such as tremors or walking difficulties.
But then they also lack norepinephrine, which hinders our autonomic system causing constipation, and blood pressure alterations.
What are the symptoms of Parkinson’s disease?
The first symptom that comes to mind is tremors, right?. Tremors are the most common manifestation of Parkinson, yes. It is a “resting tremor” which means that it gets worse when we are not using our hands, as opposed to “action tremor”.
Some people call it a “pill-rolling tremor”, because patients seem to be rolling a pill, or counting coins with their thumb and fingers. It usually starts on one side and then becomes bilateral.
Other diseases have different kinds of tremors. For example, people with essential tremor have action tremors: it gets worse when they use their hand e.g. to pour water.
Another symptoms is bradykinesia: it means slow movements. You may feel like your body works too slow. You may even get stuck in the middle of some movement. Typically, patients have a hard time to start walking, as if they froze. It can be very frustrating, for obvious reasons.
Balance problems are another common one: walking becomes extremely difficult for Parkinson’s patients. First, they find it hard to take the first step, like if the foot has stuck to the floor. Also, they tend to lean forward, so when they actually start walking, it looks as if they are going to dive and floor onto the floor.
They walk with many short shuffling steps, dragging their feet and their arms don’t swing while they walk. Their pace slows down. Sometimes they can’t stop walking when they decide to, so the fall once and again.
Patients with Parkinson suffer rigidity: their muscles are stiff. They have too much tension (that is called dystonia). Sometimes, they have curled and clenched toes, which can cause sore arms and pain.
The “not-so-well-known” symptoms
· Loss of smell: this symptom is very important because most people don’t link it to Parkinson’s disease. However, it can precede tremors for years. That’s why some scientists consider it kind of an early marker of the disease.
· Poker face: there is an important loss of facial expressions during Parkinson’s disease. You can’t tell if they are feeling sad, happy, angry…
· Small handwriting: their writing becomes small and very difficult to read.
· Slurred speech with a monotone pitch. This, along with handwriting problems, can deteriorate communication with those around them.
· Mental issues. Because Parkinson is a neurodegenerative disease, patients can suffer depression, anxiety, memory problems and delusions.
· Sleep disorders: disrupted sleep, restless leg syndrome.
· Swallowing problems: when they start is a good idea to try and find the best-tolerated foods, to avoid bronchial aspiration.
· There are some autonomic system maladjustment symptoms like constipation, blood pressure alterations (both highs and lows) and hyperhidrosis (too much sweating).
How to diagnose Parkinson’s disease
Parkinson is a difficult disorder to diagnose. There are no specific tests for it, and sometimes the early symptoms can mimic other disorders.
Which other disorders can look like Parkinson’s disease?
1. Essential Tremor
Essential Tremor looks like Parkinson’s disease because it consists of hand tremors. Unlike Parkinson’s, this tremor is more evident during movement, whereas in Parkinson’s it’s worse while resting.
Patients with essential tremor disorder usually don’t suffer other symptoms like bradykinesia, rigidity… If you have these, Parkinson is more likely.
There is a test that sometimes helps with the diagnosis: the DaTSCAN. Patients with Parkinson’s disease have an abnormal DaTSCAN while in patients with essential tremor it will be normal. It’s not 100% accurate though, there are false-positive and false-negative cases.
2. Drug-Induced Parkinsonism
Some drugs can cause Parkinsonism (same symptoms but without the disease). The main ones are antipsychotic drugs because they work by reducing dopamine levels (psychotic patients have too much dopamine, the opposite of Parkinson’s disease patients).
3. Parkinson-plus Syndromes
These syndromes share some symptoms with Parkinson’s disease, like tremors, rigidity, bradykinesia… There are several of them like multiple system atrophy, progressive nuclear palsy, corticobasal degeneration and dementia with Lewy bodies.
Each of them has some additional features that makes them different from Parkinson like early falls, dementia, hallucinations… Also, they have a worse prognosis than Parkinson’s disease and don’t respond as well to treatment.
The most useful tests for Parkinson’s disease
Clinical criteria: the 3 main symptoms of Parkinson’s disease are:
-
- Tremor at rest
- Bradykinesia (slowness of movement)
- Rigidity (muscle stiffness)
If you have 2 of the 3 symptoms, the diagnosis is very likely.
Another useful test is the DaTSCAN, although it must be interpreted carefully. As we said before, it doesn’t diagnose Parkinson but it can exclude essential tremor (which shows a negative DaTSCAN).
Another useful trick is “improvement after L-dopa”: as a test, your doctor may treat you with L-dopa or carbidopa-levodopa for a short time, to see if your symptoms improve. If your symptoms improve, it’s probably Parkinson’s.
How to treat Parkinson’s disease
Levodopa + Carbidopa
Levodopa (L-dopa) is the main drug against Parkinson’s disease. The extra L-dopa turns into dopamine, which is low in these patients. It has some side effects, like nausea, dizziness, and low pressure.
To reduce these annoying side effects, there is a combination: levodopa with carbidopa. Carbidopa decreases L-dopa conversion outside the brain so that there are fewer side effects.
· “On-Off” phenomenon
At first, there is usually good control of the disease with L-dopa + carbidopa. But after some years patients can start to experience the “on-off” phenomenon.
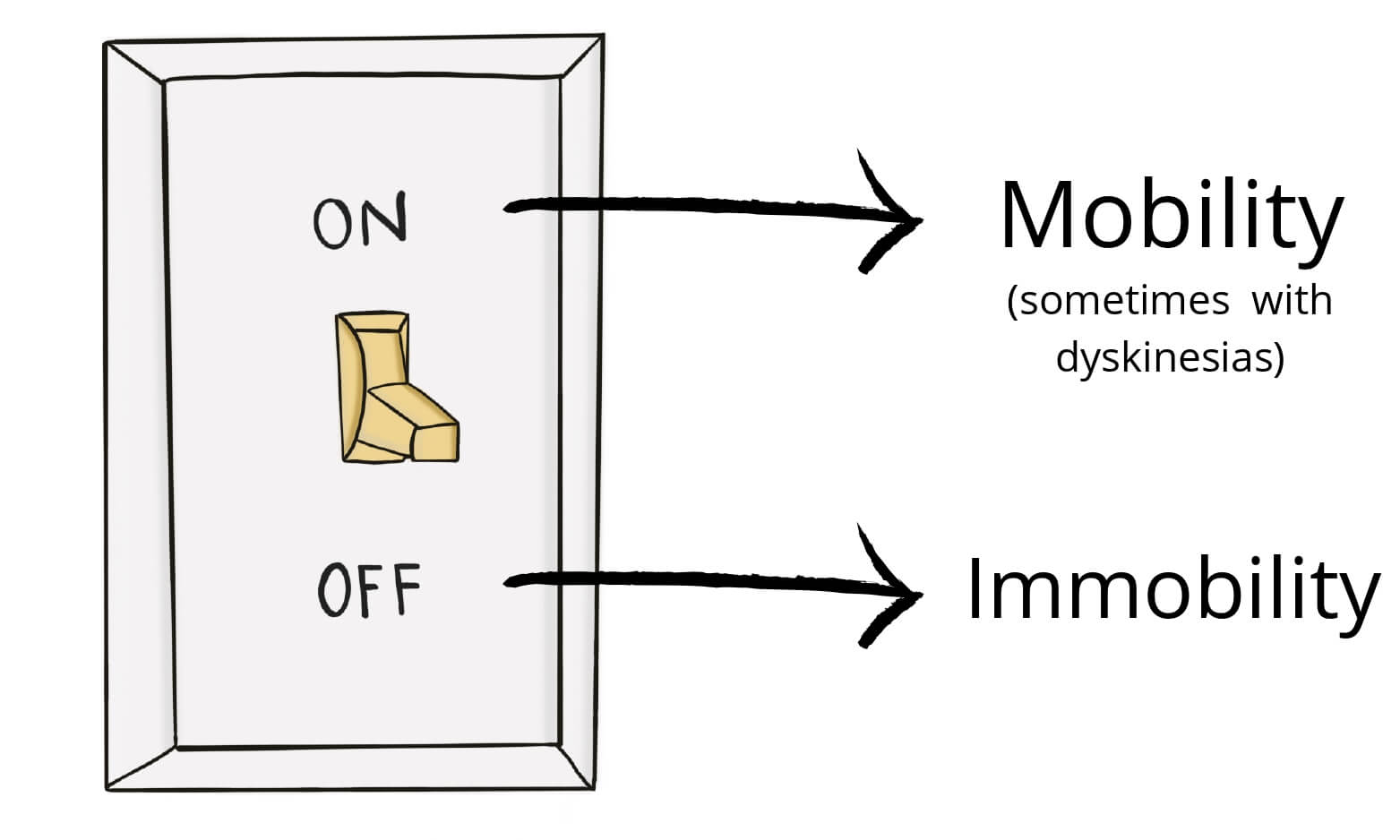
The “on-off” is like the patient has a switch with 2 positions, one of mobility (ON) and another one of immobility (OFF). The patient may be well at some point, active (ON) and suddenly, he enters the “off” position as the L-dopa effect wears off.
This usually happens some hours before the next dose. During the “off” position, the symptoms come back and the patient is bradykinetic, rigid…
During the “on” period, you may have positive symptoms. The dopamine can “kick in” too hard and cause dyskinesia (disorganized sudden movements).
- “On” period: dyskinesia (abnormal sudden movements)
- “Off” period: bradykinesia (slow movements)
Many of the other therapies for Parkinson’s disease have the role of decreasing this kind of fluctuations, like inhaled levodopa, L-dopa infusion bomb…
Inhaled carbidopa-levodopa
This route of administration is faster because the L-dopa gets directly into your bloodstream. That’s why we use inhaled carbidopa-levodopa to control fluctuations and OFF symptoms.
If the effect of L-dopa is starting to wear off and it still isn’t time for your next dose, you can take one inhaled dose for a fast (and short) improvement.
Carbidopa-levodopa infusion
This device requires a catheter directly to your duodenum.
A bomb will pour L-dopa gel into your duodenum, where it will pass to your bloodstream, avoiding the gastric metabolism. That way, you’ll get a steady stream of L-dopa, with much more stable levels and fewer fluctuations.
· Who is it for?
L-dopa infusion works best for patients that respond well to oral L-dopa but have severe motor fluctuations and dyskinesia during “on” periods.
· How does it work?
First, your doctors place a percutaneous catheter, which will enter through your abdominal skin to your stomach and to your duodenum, where the tip of the catheter will be.
The catheter is then attached to an infusion pump and a cassette where the L-dopa is stored. The pump will release L-dopa in 3 different ways:
- Morning dose: a first dose as the patient wakes up.
- Continuous dose: the pump will progressively release L-dopa throughout the day until the total required dose is met.
- Extra doses: if the patient enters an “off” period, they can push a button to get an extra dose, to control the episode.
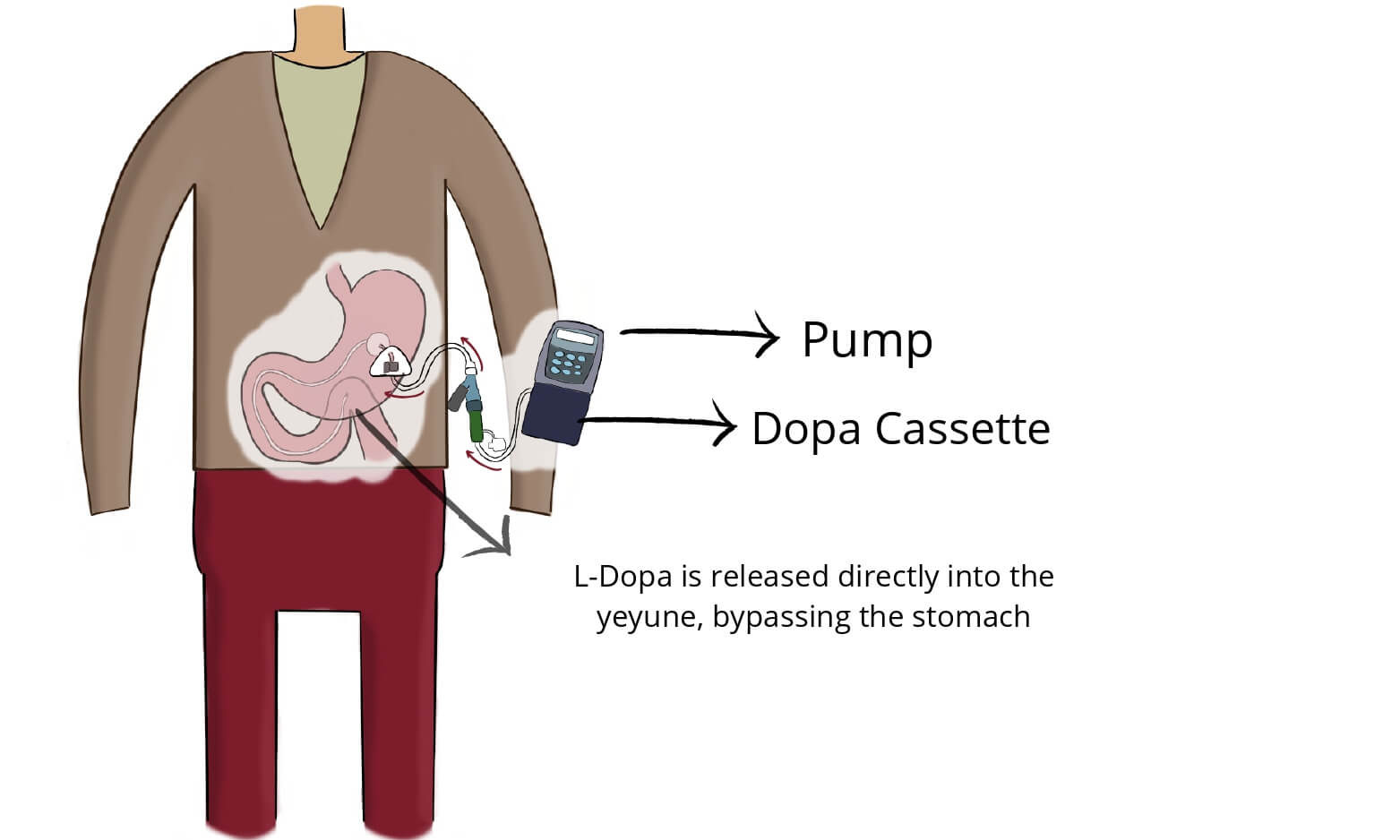
Sometimes, doctors may choose to run a test first. They can place a nasoduodenal tube (through your nose) and try it for some days, to make sure it works for you (before performing the whole procedure).
Dopamine agonists
Dopamine agonists are drugs that “look like dopamine“. They have a similar structure to dopamine, so they have a similar (but lighter) effect.
In some cases, they last longer and can decrease the on-off phenomenon. They have some unpleasant side effects like hallucinations and compulsive behaviors (hypersexuality, gambling, excessive eating…).
MAO B inhibitors
Instead of increasing the dopamine production, they decrease dopamine break-down processes, so that it lasts longer. Some patients use it along with L-dopa so that there is increased production and less breakdown (double effect).
Never mix them with antidepressants because they can have some serious side effects. Never take drugs without your doctor prescription.
Some examples are Selegiline and Rasagiline.
COMT inhibitors
They have the same mechanism as MAO B inhibitors: they decrease dopamine breakdown. They can also be used with L-dopa.
Sometimes, they can cause dyskinetic movements (too much dopamine).
Surgical procedures to treat Parkinson’s disease
Deep brain stimulation
Deep brain stimulation (DBS) is a procedure where doctors insert some electrodes inside your brain.
These electrodes are placed in very specific and precise structures of your brain. Their goal is to interrupt the disorganized activity in your brain that is causing tremors and other movement alterations.
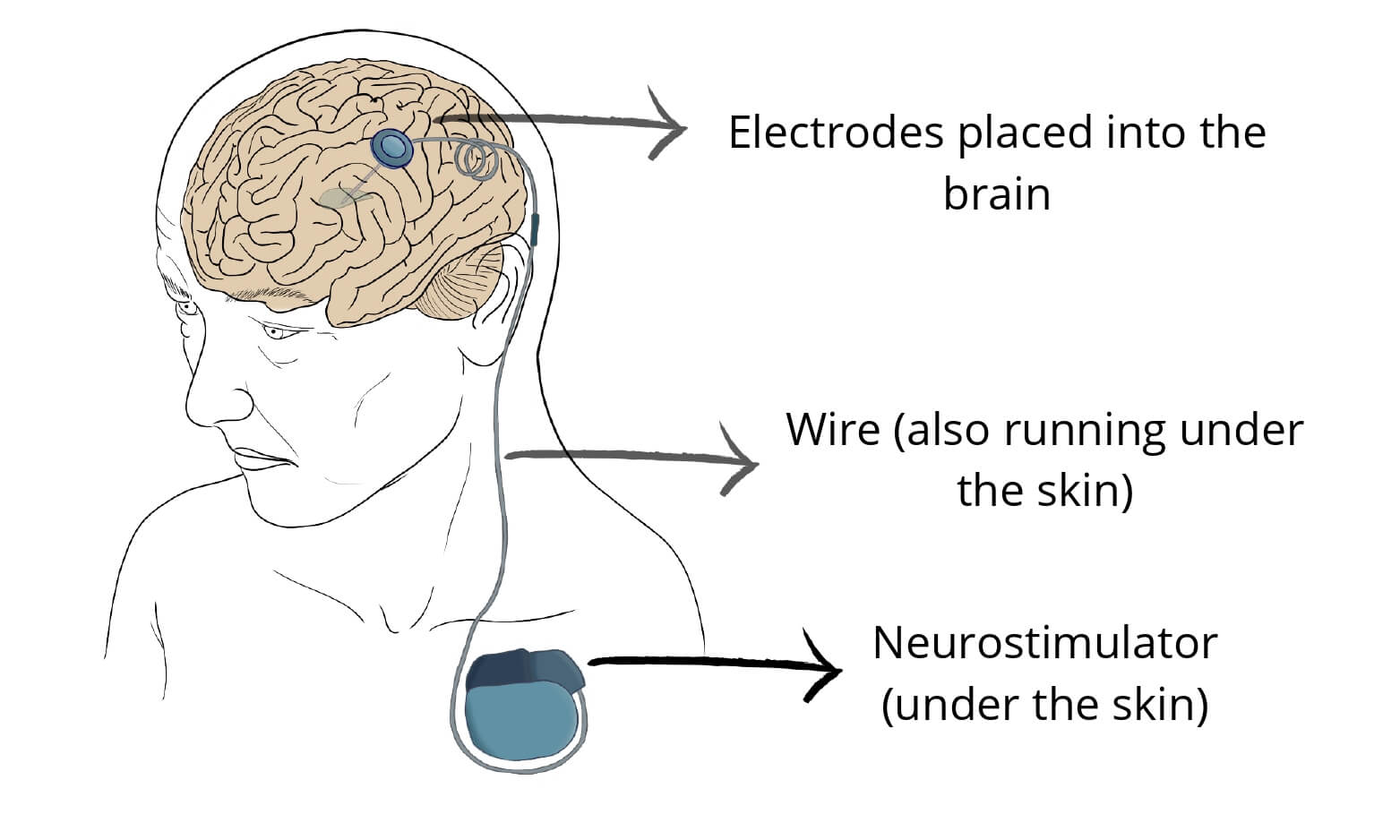
Deep brain stimulation won’t cure the disease. However, it can improve it through better control of the symptoms and lower medication doses.
Who is the best candidate for deep brain stimulation?
DBS requires careful selection of the patient. It is very useful, but only for the right patients. BDS works best for:
- Uncontrollable tremor
- Patients with good control of the disease with medication but with severe on-off phenomenon and fluctuations
- Finally, for patients that require too high doses and are limited by side effects.
BDS has the most effect on patients that respond to L-dopa. They have the same effect but DBS has a more steady effect, which allows for better control on fluctuations.
The exception is tremor: unlike the other symptoms, tremors can improve with BDS even if they don’t respond to L-dopa.
Pallidotomy and thalamotomy
The globus pallidus and the thalamus are part of the circuit in charge of fine movements (the basal ganglia). If the neurosurgeon chooses to damage some of these structures, they may interrupt some of the abnormal circuits.
These procedures are useful for patients with advanced Parkinson disease and severe fluctuations and on-off phenomenon after many years of L-dopa.
It’s also good for patients with uncontrollable symptoms. Using a special MRI, neurosurgeons will find the precise structure that is causing your symptoms.
Then, they selectively damage that structure and create a scar. That way, the electric impulse will stop (and so will the symptoms).
Sources
- General information: https://www.nhs.uk/conditions/parkinsons-disease/
- Symptoms: https://www.mayoclinic.org/diseases-conditions/parkinsons-disease/symptoms-causes/syc-20376055
- Treatment: https://my.clevelandclinic.org/health/diseases/8525-parkinsons-disease-an-overview
- Deep brain stimulation: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/deep-brain-stimulation
Leave a Reply