Multiple births are more common today than they were in the past. This is due to older women getting pregnant and the use of assisted reproductive technology. However, there are several possible complications of multiple pregnancies, more so if the fetuses are sharing the same placenta and amniotic sac.
Table of Content
What is a multiple pregnancy?
It’s a pregnancy with more than one fetuses at the same time. Not all multiple pregnancies are the same, though. There can be one or several placentas, and there can be one or several amniotic sacs.
The causes behind multiple pregnancies
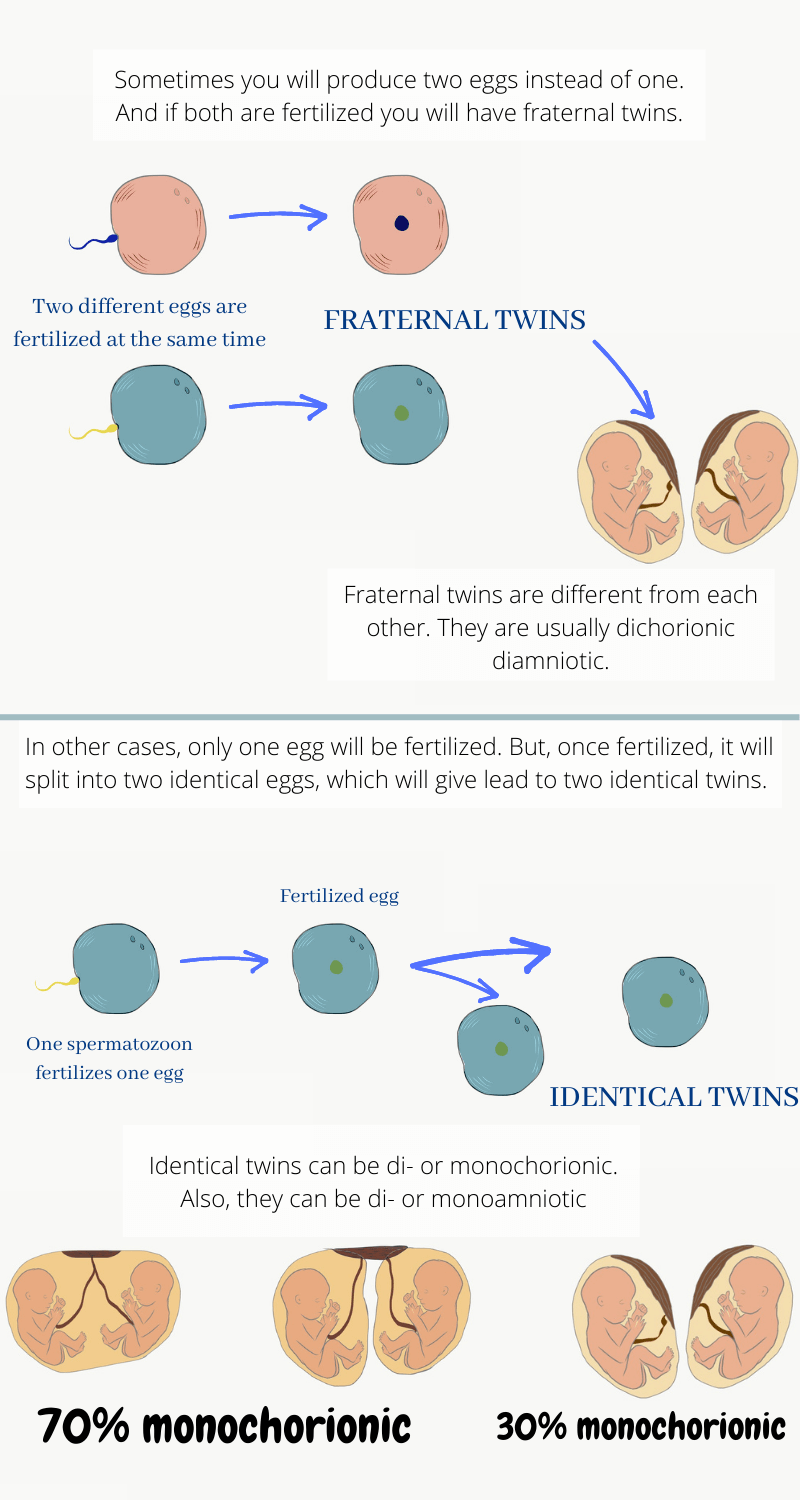
If you are pregnant with a multiple pregnancy, then there are two possible scenarios to explain it.
The first option is that you released not one but two eggs during ovulation. Then, both of them were fertilized. That is called fraternal twinning and leads to two genetically different fetuses. Each of them will have its own placenta (dichorionic) and amniotic sac (diamniotic).
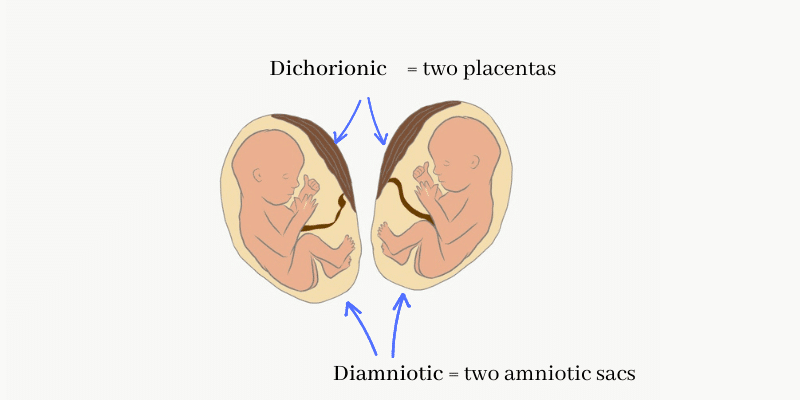
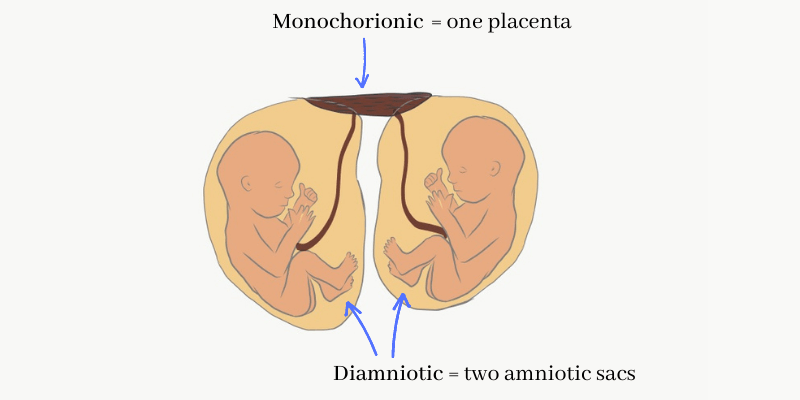
The second possibility is that only 1 egg was released and fertilized. And once fertilized, that egg split in two. This will lead to genetically identical fetuses and is called identical twinning. In identical twinning, the fetuses can be dichorionic and diamniotic like in the first example. Or they can share a placenta (monochorionic) but still have separate amniotic sacs (diamniotic).
Finally, although it’s uncommon, they can share both the placenta and the sac (monochorionic monoamniotic twins).
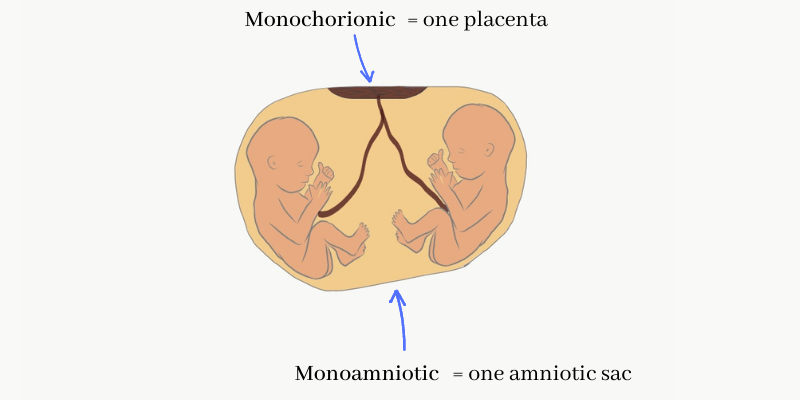
Thus, if the doctor realizes your twins are sharing their placenta then they will be identical. This can be checked during the obstetric ultrasound. However, sharing a placenta can have a dangerous downside. Babies can suffer several complications. like twin-twin transfusion syndrome, for example.
Basically, one of the fetuses takes more blood for himself than he should, leaving his brother/sister without enough oxygen and nutrients. Yes, nature can be cruel sometimes, can’t it?
Predisposing factors for multiple pregnancy
There are some factors that may make it more likely for you to have a multiple pregnancy. In most cases, the reason is you‘ll release several eggs instead of one. One of these factors is heredity: if there are other cases of multiple pregnancies in your family you’ll be more likely to have one, too. For example, if your mum has a twin brother/sister. If you are above 30, chances are slightly higher, too. Finally, the use of reproductive technology and hormones is a big factor. If you take ovulation-stimulating medicines you’ll probably produce several eggs. If all of them are fertilized that will lead to a multiple pregnancy.
Symptoms of a multiple pregnancy
Sometimes you won’t know you have a multiple pregnancy until your doctor detects it. In other cases though, you can feel some symptoms. For instance, you will gain more weight than in a single pregnancy. Also, you can feel a greater appetite and morning sickness.
Some women say they can feel “kicks” in different parts of their belly at the same time.
Anyway, the way to find out for sure is through an ultrasound/U.S. exam.
Complications Of Multiple Pregnancy
Unfortunately, multiple pregnancies involves a higher risk of some complications. These are the 10 main complications of multiple pregnancy.
1. Preterm Labors
This one is very common. Around 60% of twins are preterm. And the percentage is higher if you have more than 2 babies. Preterm labor is the one that happens before week 37. Of course, the earlier labor happens the more immature the baby will be. Very premature babies (before 28 weeks) usually require intensive care.
2. Gestational Hypertension
It’s hypertension caused by pregnancy in a woman that didn‘t have it before. It usually disappears after labor.
3. Gestational Diabetes
Similarly, it’s transitory diabetes caused by pregnancy. It also tends to resolve after labor.
4. Anemia
As we mentioned in this post it’s important to make sure you take enough iron through diet and supplements. This will decrease the risk of iron-deficiency anemia.
5. Birth Defects
There is an increased risk for some malformations such as spina bifida and other neural tube defects. Again, remember to take enough folic acid. Your doctor will tell which supplements you need.
6. Twin to Twin Transfusion Syndrome (TTTS)
It only happens with identical twins that share their placenta: that is monochorionic twins. Through abnormal vascular connections, one fetus will get more blood than the other.
The fetus receiving more blood (usually called “recipient twin”) will suffer a cardiovascular overcharge. This cardiovascular overcharge will cause congestion and polyhydramnios (too much fluid in the amniotic sac).
The other fetus (the “donor”) won’t have enough blood to grow healthy. He will be smaller, with oligohydramnios (too little fluid), and may even die.
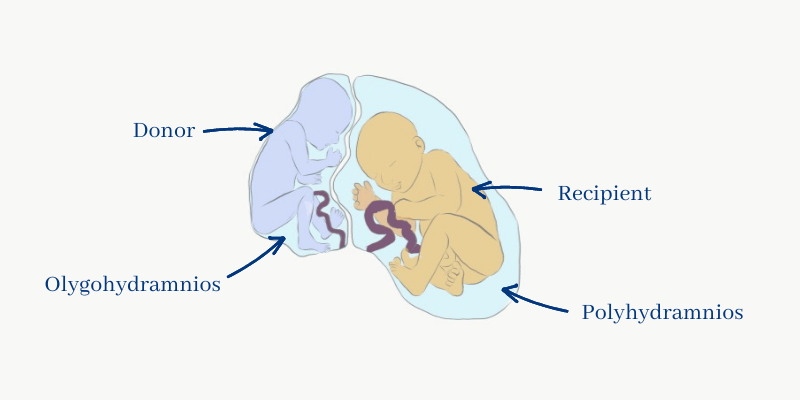
In some cases, you may need to undergo some surgery on the placenta. Sometimes, induction is the only solution.
7. Abortion/Miscarriage
After a twin-to-twin syndrome sometimes you can lose your pregnancy. There is even a phenomenon with its own name: the vanishing twin syndrome.
When it happens, your doctor will see two fetuses during the first-trimester U.S. Then, in the following U.S., there will only be 1 fetus left, as if the other one had disappeared. Indeed, the other fetus died and eventually underwent resorption.
8. Polyhydramnios
It means “too much fluid in the amniotic sac”. As we mentioned before it can be a consequence of TTTS. The recipient twin will suffer some cardiovascular overload. That will translate into increased peeing from the baby (yes, the more the baby pees the more amniotic fluid there’ll be).
If the mother has diabetes, that’s another cause for polyhydramnios. The sugar on the mother’s blood passes to the baby’s giving him polyuria (increased urine production).
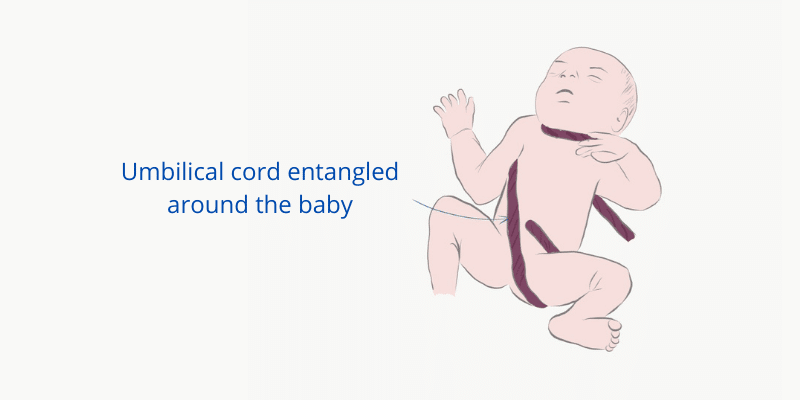
9. Cord Entanglement
When the babies share the amniotic sac, they may become tangled with each other’s cord.
They won’t asphyxiate at that moment, as they don’t breathe with their lungs (they are surrounded by fluid). They breathe through the placenta until they are born. However, if the cord compresses any structure for a long time it will injure it. For example, if it traps a hand the baby may lose it. The same can happen with their trachea.
10. Postpartum hemorrhage
Some time ago, it was relatively common for women to die from postpartum hemorrhage. Nowadays we are not familiar with postpartum bleeding because doctors know how to handle it and we assume it will be ok. But it can still happen, just only not so often.
Postpartum bleeding happens because the placenta detaches from the uterine wall, and that detachment causes bleeding. The way it usually stops is because the uterus contracts after delivery. That compresses the bleeding until it stops. Similar to when you cut yourself and press against it to make it stop.
But, if the contraction is not enough bleeding will go on. In a multiple pregnancy, there is more placental tissue than normal. And the uterus is more distended than usual. That makes it more likely to suffer a postpartum hemorrhage.
What can you do to prevent these complications of multiple pregnancy?
Increase your calorie intake. All your nutritional needs will be higher, including calories, proteins, iron, and folic acid. Make sure your diet is healthy, balanced, and complete to reduce the chances that something will go wrong.
Prenatal visits and testing. Don’t miss your appointments, there must be a close follow-up to make sure your babies are growing healthy.
Tocolytic medicines. If you start to get contractions but your babies are not fully mature, your doctor may choose to delay labor with tocolytic drugs. They will slow down and even stop contractions, to give your baby more time to develop.
Sometimes, if the babies are born before week 37, they can get hyaline membrane disease when they are born. It’s a respiratory disease that causes distress, they can’t breathe normally because their lungs are not fully developed.
To prevent it, your doctor must delay labor as much as possible. Then he will give the mother corticosteroid therapy. This speeds up the baby’s lung development.
How do you deliver multiple babies?
If both your babies are in a head-down position, a vaginal delivery is possible.
If one of them is in a head-down position but the other one isn’t, the first one may be delivered vaginally. Then, the doctor may try to reposition the second baby into a head-down position. If he succeeds, this baby too can be delivered vaginally. Sometimes the doctor won’t be able to reposition the baby and you will require a C-section.
If something goes wrong during delivery and the babies start suffering and not getting enough oxygen, you’ll need an emergency C-section, too.
Leave a Reply