Why Do We Need Cancer Stages?
Breast cancer stages are a good way to get an idea of how aggressive the tumor is and how much it has spread. Staging comes after diagnosis, and it gives us a sense of:
-
- how invasive the tumor is
- its prognosis
At the same time, this information allows us to choose the best treatment for each case.
For example, a small 1 cm tumor may be treated with just surgery. On the other hand, metastatic breast cancer will require other therapies, like chemotherapy.
About survival rates: You may read things like: “stage 3 breast cancer has a 5-year survival rate of 86%“. This doesn’t predict what will happen to a specific woman. Instead, that percentage comes from a large-population statistics. It means that women with stage 3 breast cancer are, on average, 86% as likely as women without cancer to live for at least 5 years.
Breast cancer stages go from 0 to IV, with 0 (and I) being localized tumors and IV meaning metastatic breast cancer. The higher the stage, the more advanced the tumor, and the worse prognosis it will have.
Breast Cancer Stages: From 0 to IV
Breast cancer stages can be really complex if you get into detail but a good simple overview is this:
- Stage 0: very small tumors. They are usually in situ tumors, only seen under the microscope.
- Stage 1: just a small tumor without lymph node involvement. It can be treated through surgery. Occasionally, you may also need radiotherapy or chemotherapy, to make sure there is no tumor left.
- Stage 2: the tumor is slightly larger and there may be tiny malignant cells in your lymph nodes (but not too many and not too large). It may require more aggressive surgery, like mastectomy or surgery to your lymph nodes. Also, you may need radiotherapy or chemotherapy.
- Stage 3: cancer has definitely spread to lymph nodes.
- Stage 4: there are distant metastases to other organs: your liver, bones…
In reality, breast cancer stages are a little more complicated than this. It used to be like that until 2018, but then they added some other factors. These factors made staging more complex, but also more accurate.
Today, breast cancer staging depends on these 7 items:
-
- T: tumor size, how large is it?
- N: (lymph) nodes, are they affected?
- M: are there metastases?
- ER: estrogen receptor status, does the tumor have estrogen receptors?
- PR: progesterone receptor status, does the tumor have progesterone receptors?
- HER 2 status, are there HER 2 receptors?
- Tumor grade: is it a high grade or low grade?
- * Optional: Oncotype Dx
TNM – The Anatomic Staging (how much has it spread?)
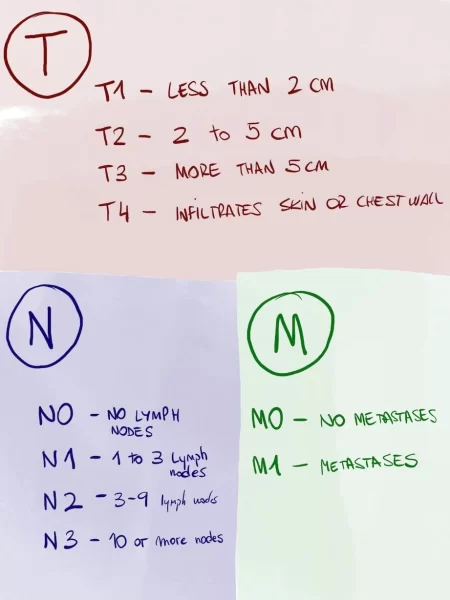
TNM stands for tumor (T), lymph nodes (N) and metastases (M).
- “T” is about tumor size. For example, if a tumor is 2 cm or less it’s a “T1”, from 2 to 5 cm it’s a “T2” and so on. The highest T is “T4“, which means the tumor is infiltrating some nearby tissue.
- “N” is about lymph nodes. If there are no lymph nodes affected you are “N0” but if there are a few nodes you are “N1”. When there are more lymph nodes you’ll be “N2” or “N3”.
- Finally, “M” stands for metastases. “M0” means there are no metastases, “M1” means there are.
Depending on the combination of size (T), nodes (N) and the presence of metastases (M), you would get a stage number from 0 to IV. This was the case until 2018, but now it’s a little more complex.
Biomarkers (what receptors does it have?)
Things changed in 2018 because of biomarkers. Doctors found that size, nodes and metastases were not the only things that mattered.
It’s also important to find out if the tumor has certain receptors. Because if they do, they will respond to certain targeted therapies. That way it would be easier to treat and you would have a better prognosis.
This was great news for patients but it required that we changed how staging was made. Breast cancer staged had to include these new biomarkers.
1. Hormone Receptor Status
A receptor is a protein on the surface of a cell. When it attaches to other molecules, it sends a signal to the cell, like “grow“. When we find these receptors on a cell we can target them to kill the cancer cell.
Breast tumors can have 2 hormone receptors on the surface of their cells: estrogen and progesterone receptors (ER and PR). Some tumors have them and others don’t.
Those tumors with hormone receptors grow faster under the influence of hormones. That sounds bad but it is not. Fortunately, we have some drugs that block those receptors, reducing the effect of hormones. Using these drugs, their prognosis gets better.
One example of “anti-hormone” drug are selective estrogen receptor modulators (SERMs). These molecules sit on the estrogen receptor and block it, so even if there is estrogen around, it can’t send the tumor a signal to grow.
Your breast cancer, then, can be:
- ER + if it has receptors; or ER – (no receptors)
- PR + it has receptors; or PR – (no receptors)
2. HER2 Status
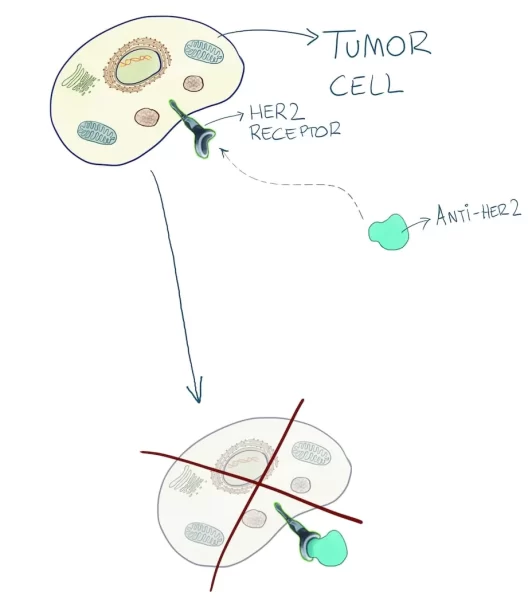
There is another protein on the surface of some tumors: HER2.
When there is a lot of HER2, that tumor grows very fast and is more likely to spread, and we say the tumor is HER2 +. If there are few HER2 proteins, the tumor grows slower and we call it HER2 -.
When we first discovered HER2, it was a sign of bad prognosis, because it meant that it would grow quickly.
However, scientists then came up with some drugs that target HER2. These drugs specifically attack cells with HER2. From that moment on, HER2+ meant better prognosis.
The most important anti-HER2 drug is Herceptin (trastuzumab).
If a patient doesn’t have estrogen receptors, progesterone receptors nor HER2 receptors, we call the tumor “triple negative“. Triple negative tumors are harder to treat when they spread, because they don’t respond to any of the targeted drugs we just talked about.
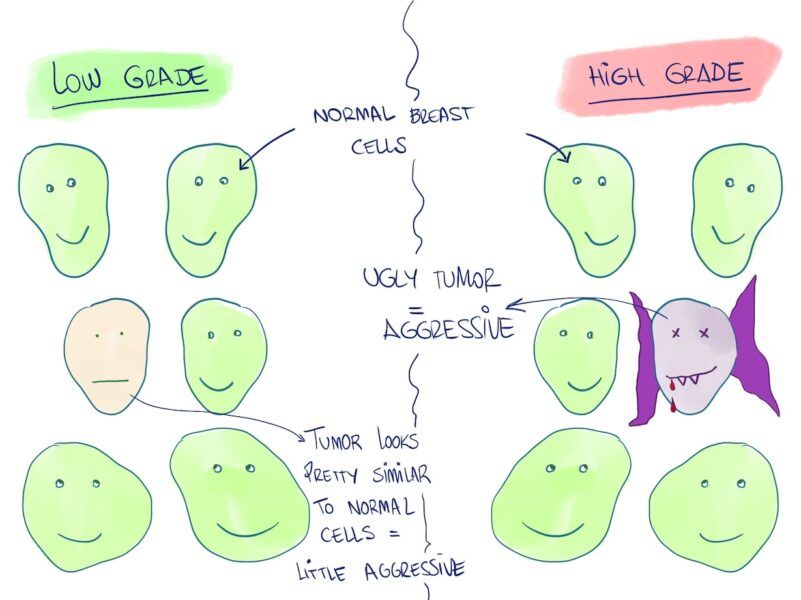
3. Tumor Grade
Tumor grade is about how the tumor looks under the microscope.
Does it look similar to normal breast cells? If so, that’s a good sign and we say it is a low grade tumor, not very aggressive.
If, on the other hand, it doesn’t look at all like normal breast cells, then that’s not so good: it’s a high grade tumor and probably quite aggressive.
4. Genomic Tests: Oncotype Dx
Oncotype Dx is a useful tool in very specific cases, mainly for women with early-stage, hormone (+), HER2 (-) cancer.
In these cases, Oncotype Dx can tell us:
- How likely the tumor is to return in the future
- If the patient will benefit from chemotherapy
Oncotype Dx works by analyzing 21 genes in the tumor. Depending on the different combinations it finds, it will figure out the chances that the tumor will come back (recurrence rate) and whether or not chemotherapy will be worth it.
You see, usually after removing a tumor, most patients get hormonal treatment for 5 years, or sometimes chemotherapy. We do this to make sure that the tumor doesn’t come back, to kill any remaining cells in their body.
However, imagine you could predict when there is very little probability that the tumor will come back. Then, after removing it, you might spare chemotherapy.
You don’t need to go though all the side effects because the tumor is already out and chances are it won’t come back. In the opposite scenario, if you have a high probability of recurrence, it makes sense that you take chemotherapy.
That’s what Oncotype Dx does. The result comes as a number from 0 to 100. 0 means it won’t come back (so you don’t need chemotherapy) and 100 means it will probable come back (so chemotherapy is advisable).
How Do All These Factors Turn into a I-IV Stage?
Finally, when we have all these data, we need to put them all together to get a breast cancer stage (0-IV). That way, we’ll get an idea of how we need to treat it:
- Is it small? surgery may be enough. Are there metastases? you will need chemotherapy, probably
- Is it hormone receptor +? We can use anti-hormone treatments
- Is it HER2 +? We can use antiHER2
There are huge complex tables that factor in all these factors and “calculate” the stage. However, that’s your doctor’s job, so don’t go too crazy looking at them because they really are knotty. They look like this:
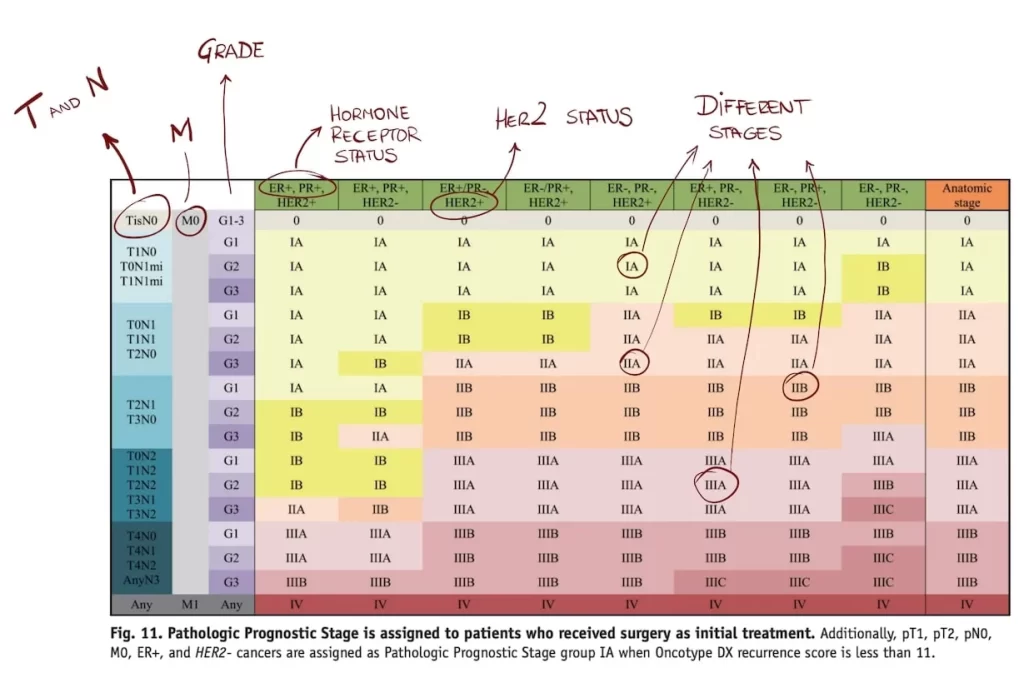
For example, imagine you have a grade 2 breast tumor that is 5 cm long, with axillary lymph nodes affected. Hormone receptors are positive and HER2 is negative. According to this table its stage is…
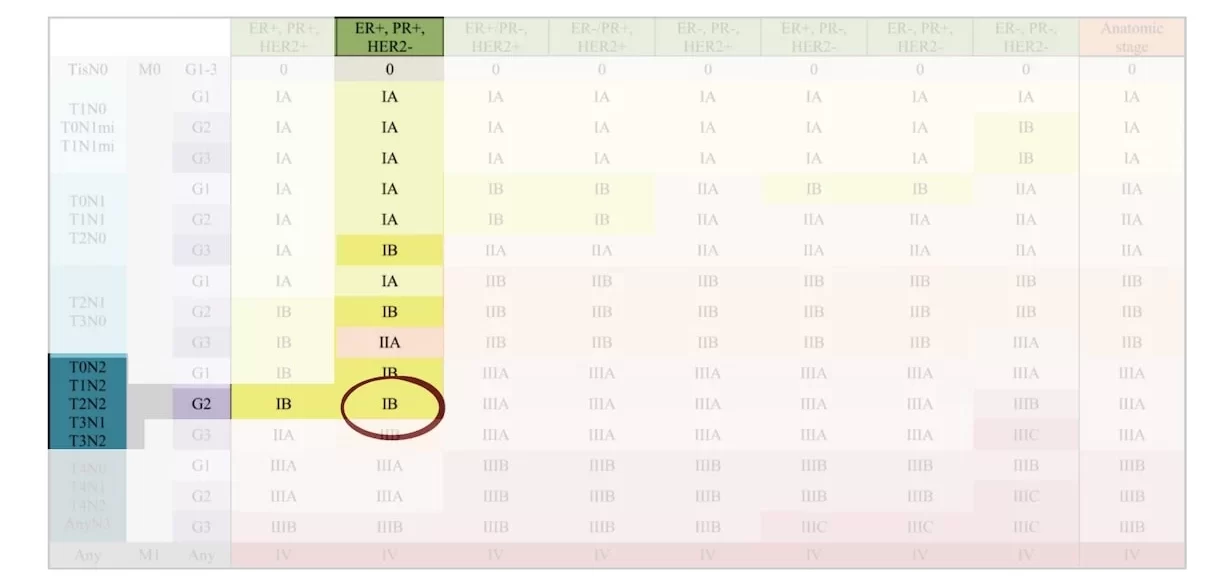
It’s a IB stage.
It’s crazy because when they added the new biomarkers in 2018, staging changed completely.
Before 2018, based on TNM, you would be a IIIB stage. Today, however, because that tumor has positive hormone receptors, you’ll be a IB stage. It went from stage III to I. Because your tumor can be treated with anti-hormone drugs, its prognosis is much better than its anatomic features suggest.
Now that staging is complete, it’s time to move on to “how to treat breast cancer“.
Leave a Reply