Alzheimer’s Disease is the first cause of dementia in the world. At the end stages, patients don’t remember even those who live with them. The last memories they keep are usually from their infancy, which may seem paradoxical… In this post, we’ll explain how to diagnose it, treat it, and what other causes of dementia there are.
Table of Content
What is Alzheimer’s disease?
Alzheimer is the number 1 cause of dementia. Around 6 million people have Alzheimer’s in the EEUU in 2021. This is devastating for the patients, but also for their families, on which it has a huge impact. If we take 10 people with dementia, over 6 of them will have Alzheimer’s Disease (followed by vascular dementia).
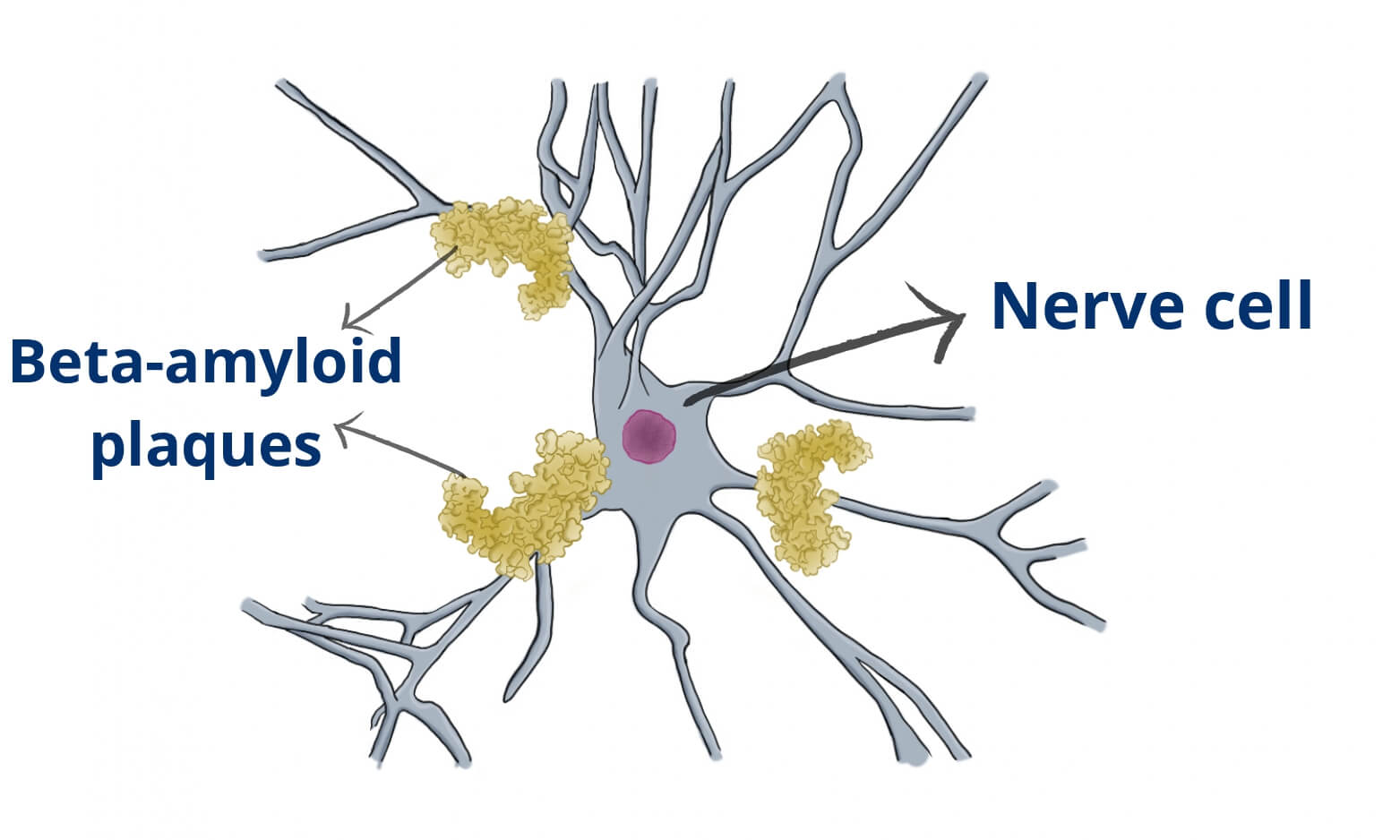
We don’t know its cause, but we know there are abnormal beta-amyloid plaques in these patients’ brains, so we think they have something to do with it. Beta-amyloid is a misfolded protein that forms plaques, which are neurotoxic. They kill nerve cells. We can find them in other diseases too, but they are typical of Alzheimer’s Disease.
Risk factors
The main risk factor is age: the older you are the higher chances for Alzheimer. Most patients get it after age 65, and the risk doubles every 5 years. As for gender, the risk is higher for women. These factors we can do nothing about, however there are others that we can control. Smoking, high pressure, obesity and alcohol seem to increase slightly the risk for Alzheimer. Alzheimer is not hereditary, although if there are family members affected, your risk may be higher.
What are the symptoms of Alzheimer’s disease?
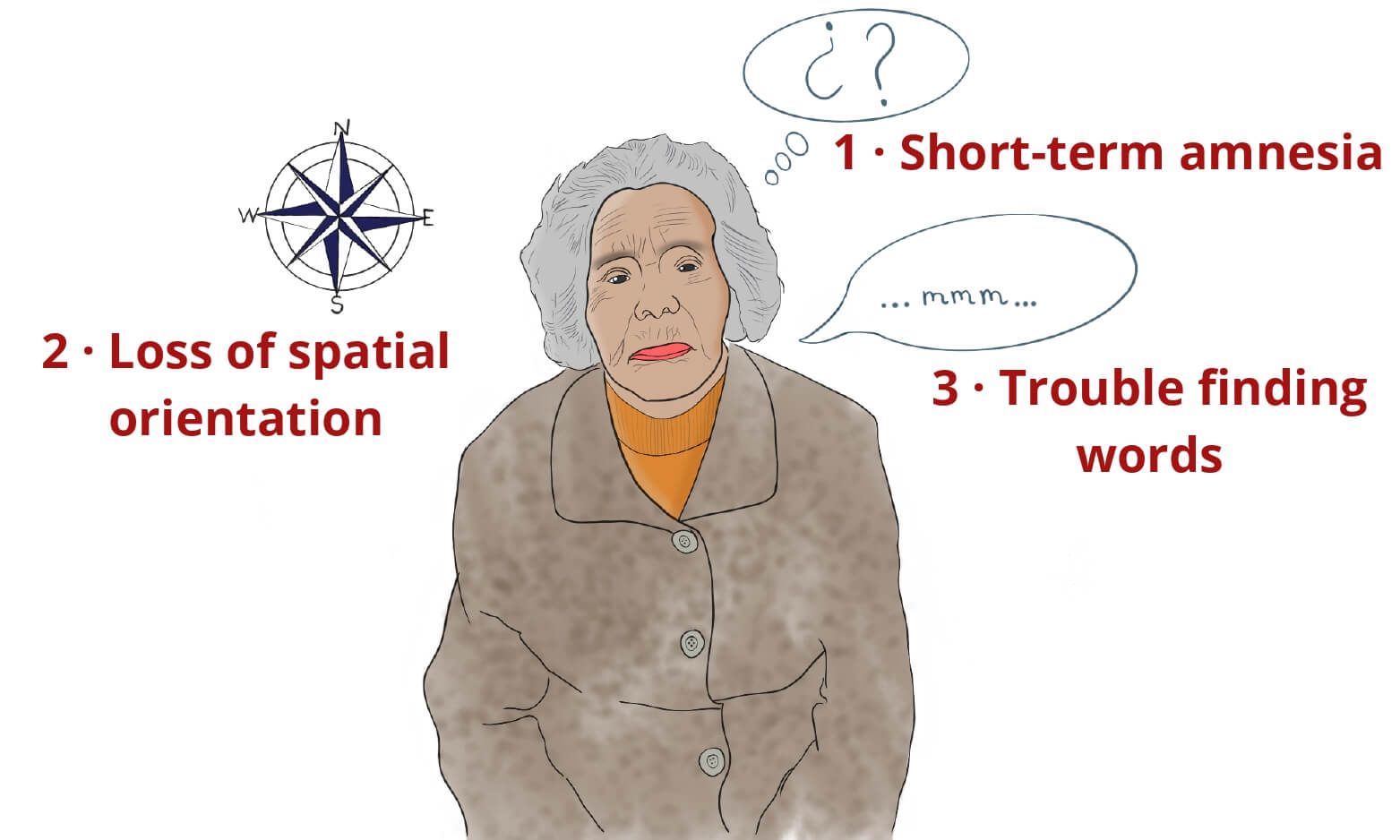
It starts with mild cognitive impairment, with small confusions. Then, it gradually progresses towards amnesia, the most characteristic symptom of Alzheimer’s Disease: you forget stuff. Alzheimer amnesia is peculiar though, it’s short-term amnesia. Patients start forgetting recent events, but they can sometimes remember past events. It’s like if the memory circuit broke from the present backwards. Patients may ask you something and 5 minutes later, they’ve forgotten about it.
However, that same patient may remember vividly some distant memories from their childhood. My grandmother was an example of this. At her end stages, she wouldn’t recognize my grandpa any more. However, one day she left us speechless telling a story from when she was little (it was a strange story, about her uncle sleeping with a gun. My mum confirmed it was true).
Another typical symptoms is language deficits, patients have trouble finding the words. Patients try to tell you something but they can’t find the right words, which is very frustrating for them. They also have a hard time trying to remember names, even from the closest family members.
Patients with Alzheimer have loss of spatial orientation: patients may get lost in familiar environments, like the grocery store, where they’ve been millions of times. Sometimes, these episodes are the first sign that something is wrong.
How is it Alzheimer different from normal aging?
It’s perfectly normal to have some memory slips as we get older (and even before that). However, it’s not normal when it impairs your normal life. If you can’t have a whole conversation, or if you get lost in a familiar space, you may consider looking for help.
How do you diagnose Alzheimer’s disease?
There isn’t a specific test to diagnose Alzheimer’s Disease, like a blood test or something similar. The most accurate test would be a brain biopsy, but nobody does it because it’s way too aggressive (it means removing a chunk of the brain and watching it under the microscope). Not an option.
That’s why the diagnosis is clinical. We search for symptoms are compatible with Alzheimer’s Disease and we exclude other types of dementia. The clinical
Your doctor has to make sure that there aren’t any other atypical symptoms that should make us consider other alternative diagnoses, like:
- hallucinations
- sudden worsening
- focal deficits (can’t move your arm, leg…)
- severe gait impairment
All these symptoms are not typical of Alzheimer’s Disease. Some of them can happen in advanced stages, but we don’t expect them in the early stages. If a patient has these atypical symptoms, we need some other tests to exclude other disorders.
What are some useful tests for Alzheimer’s disease?
As we said, there aren’t tests to diagnose Alzheimer, so most of them are good for excluding other conditions.
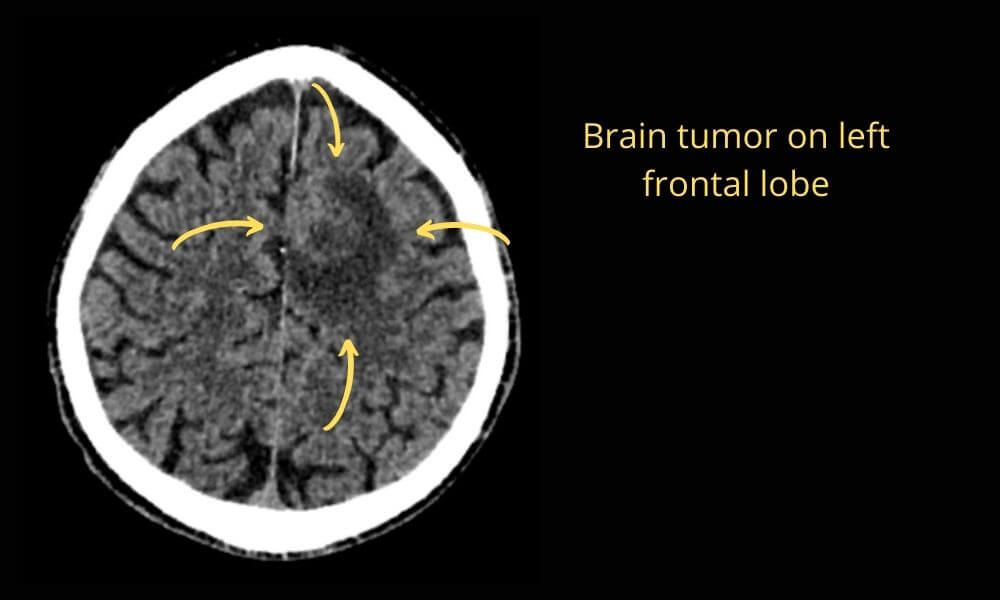
· C.T.
It’s the first imaging test to perform. It’s fast and very good at detecting:
- brain tumors
- brain hemorrhage
· MRI
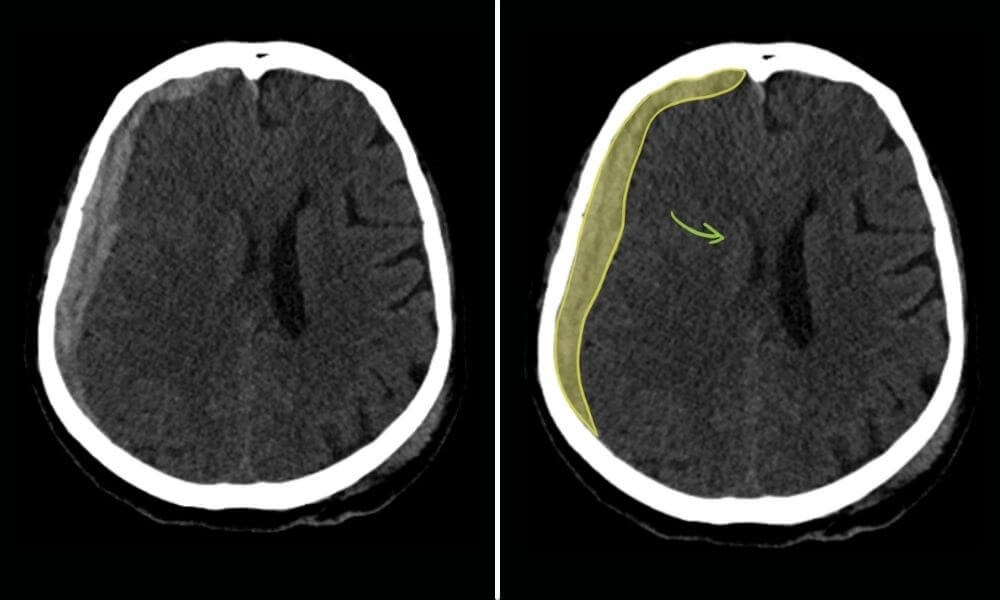
MRI is more costly and takes longer than CI. It can show us the degree of brain atrophy and it can detect region-specific patterns. For example, if we see parietal and temporal atrophy, that points towards Alzheimer’s Disease. If we see severe frontal atrophy, we can suspect another cause of dementia, called frontotemporal dementia.
MRI can also show signs of other causes of dementia, like progressive supranuclear palsy, Creutzfeldt–Jakob disease (spongiform encephalopathy) and normal-pressure hydrocephalus
· Blood tests
Some blood tests can show conditions that cause dementia, like HIV. Also, there are some live and thyroid conditions that can look like dementia. Another one is B12 deficiency.
· FDG PET
PET stands for “positron emission tomography” and FDG for “fluoro-deoxy-glucose”. This technique allows us to see the functioning cerebral brain cortex: it detects how much glucose each brain region is consuming. Using FDG PET, we can spot areas that are not functioning properly (they’ll be consuming very little glucose), which can point towards Alzheimer. It’s a complex technique, but it can detect anomalies before MRI does.
· Beta-amyloid PET
This is another type of PET. Instead of glucose metabolism, it shows deposition of beta-amyloid plaques, which are frequent in Alzheimer’s brains. Be careful though, because it’s not an accurate test: there are people with beta-amyloid deposition and no dementia (these are called false positive cases). However, if the PET doesn’t show any plaques, it’s a good negative predictor of the disease (that person won’t develop Alzheimer’s disease).
Most of the times, however, these techniques are not necessary because the patient already has typical symptoms.
So, what are other causes of dementia?
1 · Brain tumors and brain hemorrhage
Brain tumors can cause any symptom depending on where of the brain they grow. For example, if they affect the occipital cortex it will cause blindness. If they happen to affect the memory and personality areas they can cause symptoms that look like dementia. And the same goes for hemorrhage.
· How do we tell them from Alzheimer’s disease?
They have a faster course and they cause other focal symptoms.
2 · Vascular dementia
It is caused by many tiny cerebral infarctions. None of them is large enough to cause a true stroke, but they build up, causing the brain to not work correctly.
· How do we tell vascular dementia from Alzheimer’s disease?
Alzheimer’s disease has an insidious course, whereas vascular dementia happens in a stepwise fashion: every time a “mini-infarction” happens there is a worsening interval.
3 · Psychogenic dementia
It’s also called functional dementia and it happens when there is a psychological trigger. Depression can cause memory loss because patients can’t focus. In elder patients, it’s sometimes hard to tell what came first, depression or dementia.
How do we tell psychogenic dementia from Alzheimer’s disease?
If the main symptoms are anxiety and/or depression, chances are it is functional dementia.
4 · Normal Pressure Hydrocephalus (NPH)
It happens because of abnormal pressure in the cerebrospinal fluid (CSF) in the brain. It is a very important cause of dementia because it is treatable. Some patients with severe NPH will benefit from a shunt that’ll drain some of the extra CSF. The results can be astonishing: some patients are not able to walk before the procedure and then, after a few hours, they can walk again perfectly on their own.
How do we tell Normal Pressure Hydrocephalus from Alzheimer’s Disease?
Patients with Normal Pressure Hydrocephalus have these 3 well-defined symptoms:
- Dementia
- Gait impairment: they have Parkinson-like symptoms. [link]
- Incontinence: patients can’t hold their pee.
If a patient develops these symptoms in a short time of time, we should be concerned about Normal Pressure Hydrocephalus.
5 · Rapidly progressive dementia
There are some causes of dementia that have a very rapid course, like:
- Jakob-Creutzfeldt disease
- Dementia with Lewy bodies
- Progressive Supranuclear Palsy
How do we tell rapidly progressive dementia from Alzheimer’s disease?
There is a sudden worsening in the patient.
Is there an effective treatment for Alzheimer’s disease?
So far, there weren’t any effective therapies for Alzheimer’s Disease. Instead, there are some drugs to help manage symptoms.
· Cholinesterase inhibitors: galantamine, rivastigmine, and donepezil
We use them for mild and moderate Alzheimer’s Disease. They reduce the breakdown of acetylcholine, which has a role in memory and thinking. These drugs can improve symptoms for a while, but they don’t slow down the disease.
· Memantine
It’s an N-methyl D-aspartate (NMDA) antagonist, which regulates glutamate. It can improve symptoms but it won’t slow down the disease either. We use it for moderate to severe Alzheimer’s Disease.
· Aducanumab: the newest therapy
In June 2021, the FDA approved Aducanumab in the EEUU as the first disease-modifying disease against Alzheimer’s Disease. It works against beta-amyloid plaque accumulation. To use it, you need to make sure that you have beta-amyloid plaques, so you’ll need a positive beta-amyloid PET.
However, the FDA approved it through their Accelerated Approval Program. Because so far there was no effective therapy against Alzheimer’s Disease, they approved it before the phase 4 clinical trial. So we know it is safe, and we know it acts against plaques, but we still don’t know if it will effective (will it improve patients’ symptoms/disease?). There will be a large phase 4 clinical trial as patients start using it.
The decision was controversial because some people think its benefit will be minor. However, it is the first drug that could improve the disease course (hence its importance).
Update August: Things are not looking good for aducanumab. Outside of EEUU, other countries have rejected aducanumab: they consider the risk/reward ratio is not worthy. There have been some cases of brain hemorrhage while the clinical benefit is still not clear. Apparently Canada, Australia, United Kingdom, and the European Medicines Agency have rejected it.
Common questions
· Can Alzheimer’s disease kill you?
It doesn’t kill you directly, but it may shorten your life expectancy due to complications. For example, patients with advanced Alzheimer’s can have trouble swallowing, which makes them prone to bronchoaspiration pneumonia.
The average patient lives around 5-10 years after the diagnosis, but it depends on each person. Some patients live up to 20 years.
· Is Alzheimer’s disease inherited?
It is not inherited from parents. However, there is a genetic component, which means there is a slightly higher risk for family members.
· Does MRI show Alzheimer’s disease?
We can’t diagnose Alzheimer’s disease with MRI, but it is useful to rule out other disorders. Also, it shows the degree and location of brain atrophy: if there is marked atrophy of the temporal lobe, it’s an indirect sign of Alzheimer’s.
Sources
- Lifestyle and dementia: https://www.cdc.gov/aging/publications/features/healthy-body-brain.html
- Treatment: https://www.nia.nih.gov/health/how-alzheimers-disease-treated
- Aducanumab: https://www.neurologia.com/articulo/2022072
Leave a Reply