Believe it or not, there are still many taboos when it comes to doctors. Believe it or not, some doctors are not used to talking about certain topics, like your gynecological health.
If doctors aren’t comfortable with those conversations, women won’t be either.
That makes it difficult to talk about things like menstruation or sexual health.
But that’s not how things should be. We should be able to discuss gynecological issues in the same way as anything else.
And that’s what brings us here today: let’s see those taboos that are too sensitive to talk about.
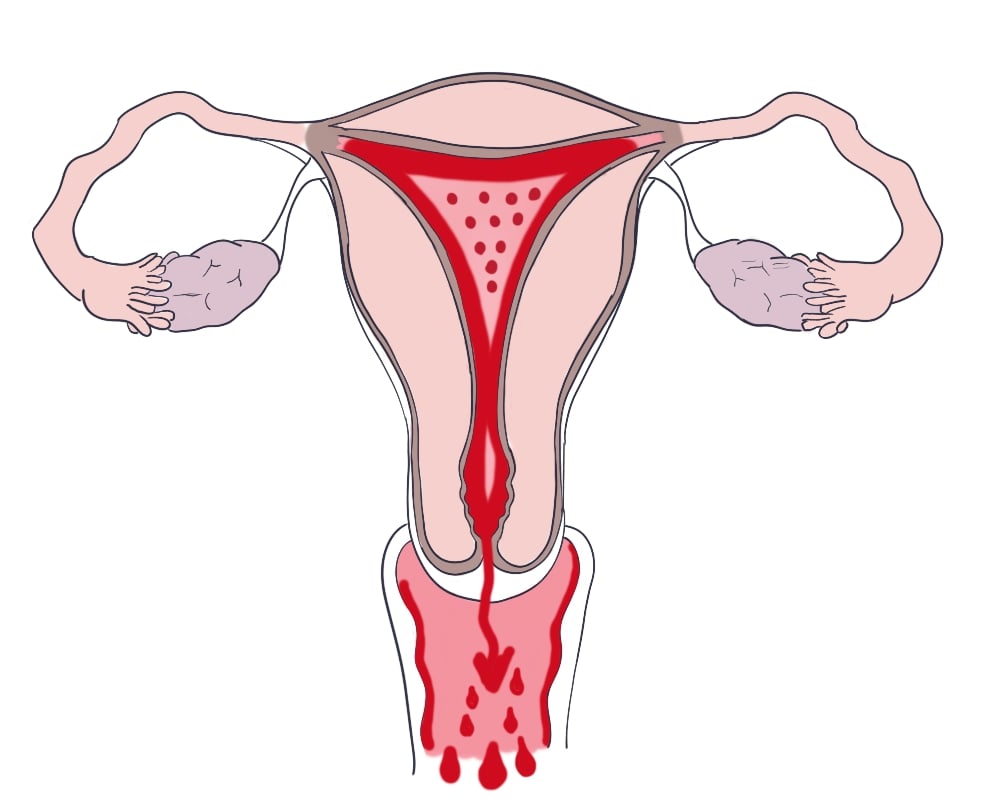
Menstruation
Menstruation is still a taboo in many cultures. Throughout the world, many young girls don’t know about menstrual hygiene and what to do for the pain.
They avoid discussing it because they are too embarrassed.
When you have your first period, it’s essential to know how much pain is considered “normal“. Also, somebody should warn you of the emotional changes that usually come with a period.
Vaginal health
We’re talking about infections, odor, and discharge. In some contexts, these things will be considered “gross,” so don’t even think about talking about them.
If you do, be ready to take the consequences. So, how the hell are you supposed to learn what’s normal and what isn’t?
Sexual Health
Contraception, sexually transmitted infections (STIs), and safe sex practices… Sexual health issues are difficult to talk about, especially in conservative settings.
And it is a big one.
Nobody should get an STI or an unwanted pregnancy just because they have no one to talk to.
I think it’s time doctors and society start facing these conversations like grown-ups.
Menopause
“– Menopause? Get out of here! Just go through it and shut up.”
Menopause is a natural phase in a woman’s life. However, it can come with different physical and emotional changes.
Many women avoid discussing hot flashes, mood swings, and sexual desire due to the stigma.
Pelvic floor health
After giving birth, many women suffer incontinence and pelvic prolapses.
Yet, bringing them up can cause embarrassment and fear. But it shouldn’t be that way because they are very common and, often, they are treatable.
So, if you don’t seek help, you may miss out on possible solutions.
This one has improved over the last decades, though. In our parent’s generation, no one would even talk about the pelvic floor. Nowadays, it’s much more common for women to know about Kegel exercises.
Gynecological exams
Some women find it violent to have a pelvic exam, especially if it’s done by a man.
Avoiding tests such as Pap smears and pelvic exams is a mistake. Those tests detect some conditions at an early stage so that we can treat them early.
If you miss this opportunity, it may be too late by the time you finally decide to get a diagnosis.
So, please make sure you don’t miss your regular screenings.
Female sexual pleasure
Nobody likes talking about this stuff with their doctor.
Of course, if you have an older sister or older friends, they’ll tell you about it. But what if you don’t have them?
Then, a gynecologist should be able to help you understand because that’s what they know about.
Many doctors focus on specific disorders, e.g., breast cancer or endometriosis. They will tell you they are not sexologists.
Well, then you need to find a new doctor.
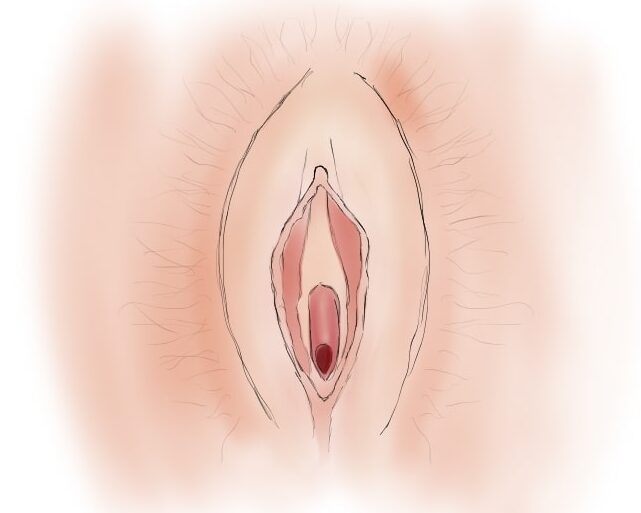
Body image and vulva diversity
Many women feel self-conscious about their genitals’ appearance. After all, we are exposed to unrealistic beauty standards all the time.
Many women are ashamed of their vulva, not knowing there are thousands of women thinking the same.
Not everybody looks the same, and that’s true for your face, your body, and, of course, your genitals.
8 common myths
Myth 1: Vaginal Odor Means Infection
Not every vaginal odor means an infection.
Your vagina has a natural odor that can vary throughout the menstrual cycle.
If you have a strong, fishy odor, then yes, it might be a sign of an infection, like bacterial vaginosis.
But mild changes in smell are often normal, and you shouldn’t worry.
Myth 2: Using Tampons is Not Safe
Some women are afraid to use tampons because of Toxic Shock Syndrome (TSS).
TSS is a rare condition that may happen after tampon use. Yet, it only happens if you don’t use them the right way, leaving them inside for too long.
Just be sure to use your tampons correctly and change them as instructed. That way, you’ll be safe.
Myth 3: Pap Smears Detect All Gynecological Issues
Pap smears are great at detecting cervical cancer but not other gynecological diseases.
Thus, some women assume that if their Pap smear is negative, they’re free from any issues.
Remember, Pap smears don’t screen for other conditions like ovarian cancer or STIs.
Myth 4: Birth Control Causes Infertility
Birth control methods do not cause infertility. Not even long-term ones like IUDs.
Most birth control methods are reversible. After you stop using them, you can get pregnant again.
The only exception is tubal ligation and vasectomy, which are harder to revert.
Myth 5: Douche Cleanses the Vagina
Some women believe that douching cleans the vagina. It doesn’t. It disrupts its pH balance, leading to infections.
Your vagina is self-cleaning and doesn’t need douching.
Myth 6: Period Pain is Always Normal
If you have severe pain during your period, then something might be wrong.
It’s okay to feel some mild discomfort, but it shouldn’t disrupt your everyday life.
Conditions like endometriosis can cause severe pain.
Myth 7: Tightening Products Restore Vaginal Tightness
Some products claim to restore vaginal tightness after childbirth.
Don’t use them: they don’t work and can even be harmful.
Your vagina expands during arousal and childbirth. And these products won’t change that.
Myth 8: You Can’t Get Pregnant on Your Period
Chances are lower, yes. But it’s still possible to get pregnant during your period.
Sperm can survive for several days inside the body, so you never know 100%.
Myth 9: Painful Intercourse is Normal
Intercourse shouldn’t be painful.
Some conditions can cause pain during sex, like vaginismus, infections, or endometriosis.
Myth 10: Menopause Means the End of Sexual Desire
Menopause doesn’t mean a complete loss of sexual desire.
It does bring hormonal changes, but you can still maintain a satisfying sex life.
The key? Have open communication with your partner and address any physical discomfort you have.
Leave a Reply